Special Message to Men Whose Partners Have Had or May Have a Tubal Ligation
Some men would like to have a vasectomy even though their primary sexual partners (wives, fiancées, or long-term girlfriends) have already undergone bilateral tubal ligation, otherwise known as "BTL", "tubal", "tubal ligation", "tubes tied", or "female sterilization". There are a number of reasons for this:
1. A man may have one or more partners in addition to his primary
partner and he does not want to get her/them pregnant.
2. Both members of a couple may wish to undergo sterilization as part of
a pact to demonstrate their commitments to each other.
3. A couple may fear that a tubal provides inadequate protection
against unwanted pregnancy. They may have an
acquaintance who became pregnant after a tubal.
The first reason is adequate justification for vasectomy, with the intended goal (avoidance of pregnancy with outside partners) being worth the risks of vasectomy.
The second reason is not MEDICALLY justifiable. That is, the risk of pregnancy after either vasectomy or tubal ligation is so low that the risk of either procedure is probably greater than the risk of pregnancy after either procedure. In the couple's minds, the two procedures may be SOCIALLY justifiable, but the second procedure does pose an unwarranted medical risk. My suggestion to such couples is that if they want to demonstrate their commitments to each other, an alternative method, such as simultaneous tattoos, would be less risky.
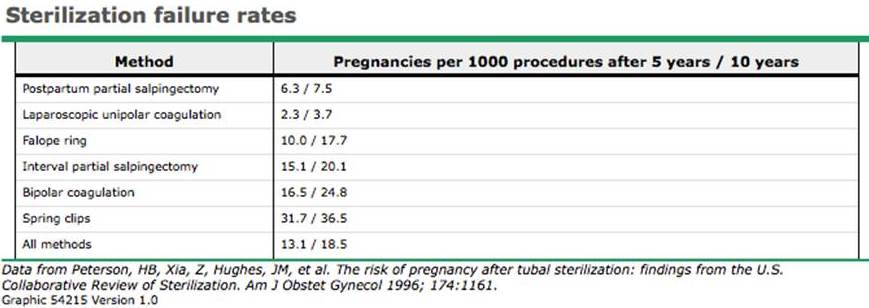
The third reason may be medically justifiable. One must compare the risks of vasectomy with the risk of pregnancy after tubal ligation. Data varies about both risks. See the table below.
CERTAINLY a tubal after a vasectomy is not justifiable, unless a woman has extramarital partners. A vasectomy (A) is less risky than a tubal [tubals are performed under general anesthesia and involve entry into the abdomenal cavity], (B) has an extremely low failure rate, and (C) can be easily monitored periodically by simply having a qualified person in a lab look at a semen specimen under a microscope for the presence or absence of sperm. The exception to "A" is the tubal performed as part of a scheduled Caesarean section. If a man with a pregnant partner due to have a C-section (because of large twins or prior C-section) is considering vasectomy, he should delay vasectomy until after the birth. If his partner does have a C-section and undergoes tubal ligation during that C-section, he should NOT have a vasectomy, because the risk of vasectomy outweighs the risk of pregnancy after the BTL.
Is vasectomy after a tubal warranted to decrease the risk of unwanted pregnancy? That depends on the technique used for the tubal and the track record of the vasectomy provider. The risk of vasectomy (post-procedure bleeding, infection, or chronic pain), albeit low, may be comparable to the risk of pregnancy after BTL, depending on the technique used for the BTL. It is true that depending on the techniques used, tubals fail more frequently than vasectomies. It is true that tubals cannot be monitored for effectiveness as easily as vasectomies. To monitor a vasectomy, one need only submit a semen specimen for microscopic analysis for the presence or absence of sperm, a test which is inexpensive and carries NO RISK. But to monitor a BTL (to determine whether the tubes have "grown back together"), a woman would have to undergo an X-ray test called a hysterosalpingogram (HSG), during which contrast is injected into the uterus to see whether it passes into and through the tubes. An HSG is expensive and carries the risks of radiation exposure and infection, so it is almost never performed to monitor tubal effectiveness. It is true that when pregnancy occurs after vasectomy, it is usually a healthy uterine pregnancy. In contrast, when pregnancy occurs after BTL, half are ectopic (outside the uterus and usually within one of the tubes) and represent a surgical emergency because they can rupture and the woman can die (though death is very rare in communities where good health care is readily available). So for a number of reasons, vasectomy is preferable to tubal ligation as a form of sterilization. But if your partner has already had a tubal ligation, the risk of vasectomy may be greater than the risk of pregnancy after tubal ligation. If the fear of pregnancy after tubal ligation (the fear of tubal failure) is so unsettling that you do not enjoy sex, vasectomy is justifiable to relieve that fear.
For those who want more detail: keep in mind that
tubal ligation can
be performed at three different "times" using
one of a number of "techniques". Those
"times" are:
1. At the time of Caesarean section. The abdomen is already opened to
deliver the baby, and the tubes are simply clipped or
tied or cauterized
(burned), sometimes with a section of each tube removed between the
clipped, tied, or cauterized
ends.
2. One day after vaginal delivery. The woman is taken down to the
operating room. Her uterus is still large and the tubes are still up
around the umbilicus (belly button) before shrinking back down into the
pelvis. So, under general anesthesia (the
woman is put to sleep), a small incision is made just under the
umbilicus. Through this opening, the gynecologist lifts a section of each
tube in turn and clips, ties or cauterizes it, sometimes with removal of
a section.
3. At a time unrelated to giving birth. A woman goes to a hospital or
outpatient surgery center and undergoes tubal ligation either through a
single small "bikini" incision or "laparoscopically" with scopes and
instruments placed into the abdomen through 2 or 3 tiny openings. The
laparoscopic approach always requires general anesthesia because the
abdomen is inflated with gas so the surgeon can look around. The
bikini
incision approach is almost always performed under
general anesthesia in
countries with generous resources, but in countries with limited
resources, it is often performed under local anesthesia
administered with a needle. Under local anesthesia, It hurts when
the surgeon lifts the tubes, but thousands are performed under local
anesthesia every day in developing countries. These methods may not be
possible for women who have already had pelvic surgery, in which case
scarring may prevent the surgeon from finding or manipulating the tubes.
At any "time" of tubal ligation, the procedure can be performed using
one of various "techniques" to block the tubes. Here is a
chart of the failure rates of those techniques: