VASECTOMY REVERSAL 101 ...
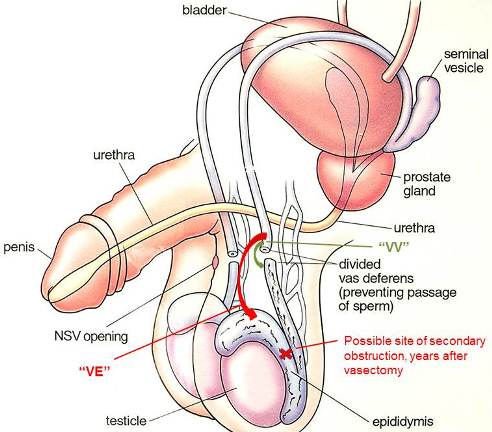
After vasectomy, sperm are still made by the testes, but since the vas tubes have been blocked, they cannot exit in the usual way. On each side, sperm can still enter the epididymis (the very long coiled tube behind the testis where sperm normally become mature) and the lowermost portion of the vas tube upstream from the obstruction imposed by the vasectomy. After vasectomy, the very fine tubes of the epididymis can become blocked. There are two possible explanations for this.
In the epididymis, white blood cells in the normal testicular circulation ingest and recycle the trapped sperm. This increased white blood cell activity is a chronic inflammation by definition. Inflammations can lead to scarring, and scarring in a very fine tube like the epididymis can cause obstruction. For example, inflammation of the liver (hepatitis) can cause scarring of the liver (cirrhosis); inflammation of joints (arthritis) can cause scarring with stiffness and decreased range of motion. The longer the duration of the inflammation, the greater the likelihood of scarring and obstruction, and this can occur in the epididymis, just as it can in any organ.
An alternative explanation for obstruction in the epididymis after vasectomy is that pressure increases upstream from the vasectomy site and can cause a "blowout" in the fine tubes of the epididymis, resulting in leakage of sperm and local inflammation and blockage.
Whatever the explanation for the obstruction in the epididymis (scarring or blowout), its likelihood is roughly proportional to the number of years that have gone by since the vasectomy. After an interval of only 1-3 years, the epididymis is rarely blocked, but after an interval of 20 years, the likelihood of secondary obstruction may be over 30%. Fixing the vas where it was divided at the time of the vasectomy (vasovasostomy or "VV") will not correct the secondary obstruction upstream in the epididymis. That requires a more elaborate procedure called a vasoepididymostomy or "VE", in which the portion of the vas tube above or "downstream" from the vasectomy site blockage is connected to the portion of the epididymis "upstream" from the secondary obstruction.
 "VV" vs. "VE" ...
"VV" vs. "VE" ...
Vasovasostomy (VV) and vasoepididymostomy (VE) are very different operations. Since the aim of VV is to reconnect the vas where it was severed at the time of vasectomy, it is a true "reverse vasectomy". A VV can often be performed by lifting the vas tubes out of the scrotum through a small incision, just as they were lifted out at the time of the vasectomy. The vasectomy site will be either a gap or a nodule (lump), but either way, the objective is to freshen the ends on either side of the vasectomy site and suture them back together. Left and right sides can usually be repaired in turn through the same 1/2- to 1-inch vertical incision in the center of the scrotum, all under local anesthesia in a doctor's office. The procedure is performed under magnification using optical loupes or a microscope, 10 -18 sutures are used on each side, and it takes 3-4 hours.
A VE is different in a number of ways. (1) Since the epididymis is attached to the testes, VE requires delivery of the testes, that is, the testes must be taken out of the scrotum while the connection between the epididymis and vas is made. This requires an incision larger than that needed for VV. (2) Also, the portion of the vas between the vasectomy site and the epididymis is not used, so the gap that must be bridged is longer, requiring that the upper section of vas be "mobilized" to provide the needed length. In order to do this, the surgeon must usually make two incisions, one left and one right, which can be extended up toward each groin to allow for dissection and loosening of higher portions of the vas. (3) Finally, the epididymal tubes are much smaller than the vas tubes. A microscope must be used, the connection between vas and epididymis (VE) is often not as strong as the connection between vas and vas (VV), and the success rate of VE is not as high as the success rate of VV. A VE is more technically demanding than a VV, and some surgeons who are excellent at VV's may not perform VE's frequently enough to be comfortable with them.
Most doctors would agree that delivery of the testes through bilateral (both sides) incisions is beyond the scope of an office environment and that general anesthesia and a formal operating room in a hospital or ambulatory surgery center should be used. In addition, since the success rate (return of sperm to the semen) with bilateral VE is only about 65%, one should consider using a surgical facility in which sperm can be harvested, evaluated and frozen at the time of the VE so that sperm is available for in-vitro fertilization if the VE fails. Saving sperm at the time of VV is much less practical for two reasons: (1) the sperm seen at the time of VV are usually not motile (active) and therefore not acceptable for freezing and in-vitro fertilization, and (2) the success rate of VV when sperm are seen coming from the lower end is very high.
| VV | VE | |
| Testes | not seen | must be delivered |
| Gap length | usually short | usually long |
| Incisions | one, short, midline | one or two, longer, left and right |
| Magnification | loupes or microscope | microscope necessary |
| Anesthesia | local works fine | general advisable |
| Procedure location | office or operating room | operating room |
| Sperm storage | not practical | advisable |
| Fees | surgeon | surgeon, anesthesia, facility |
Which men need a VE?
Ah ... that's the big question. We know that the longer the interval in years between vasectomy and reversal, the greater the likelihood of a secondary obstruction in the epididymis. But some men have secondary obstruction after only two years and some do not have it after 30 years. Wouldn't it be nice if we could determine with certainty which men need a VE before they have their surgery? Unfortunately, we cannot - not by physical exam, ultrasound, CT or MRI.
Physical Exam
There are a few clues on physical exam: (1) An epididymis that is very enlarged, firm, and tender is more likely to be obstructed than one which is small, soft, and non-tender. (2) A nodule (lump) at the vasectomy site may be "sperm granuloma", a place where sperm leaking from the lower end of the severed vas are being recycled. If the inflammation needed to recycle sperm is taking place at the vasectomy site, it is not taking place upstream, thereby sparing the epididymis and reducing pressure within it. So a vasectomy site lump is a good thing, but not all lumps are granulomas ... some are just knots of the suture or clips used during the vasectomy. (3) Some surgeons believe that high (away from the testes) vasectomy sites are a good sign ... more vas on the testis side of the vasectomy site to absorb the back pressure.
Operative findings
When the vasectomy site is investigated and the lower end is freshened, the fluid that may drain from the lower end is an important clue. If the fluid contains sperm, the likelihood of an upstream obstruction is very low and the likelihood of sperm reappearance in the semen after VV is very high. If the fluid contains no sperm, especially if it is thick or creamy and packed with white blood cells (pus cells), the likelihood of an upstream obstruction is very high and the likelihood of sperm reappearance in the semen after VV is very low. No fluid at all is a relatively poor sign, and watery fluid, even though devoid of sperm, is a relatively good sign.
To solve the dilemma ...
There are three approaches to vasectomy reversal:
(1) A surgeon may perform a bilateral VV through a single incision in the office or in a facility, regardless of the lower end fluid findings, because (a) most patients have good lower end fluid findings and do not need a VE, (b) some patients enjoy return of sperm to the semen and cause a pregnancy even when lower end findings are adverse, and (c) VV's are technically less demanding and more likely to remain open than VE's.
(2) A surgeon may perform all reversals under general anesthesia through two incisions in an operating room with a lab ready to accept sperm for storage. By delivering the testes, the surgeon can work with excellent exposure and go right to a VE on one or both sides he or she feels that fertility would be better with a VE.
The problem with approach number 1 is that when there is epididymal obstruction on both sides (which occurs about 17% of the time on average), the procedure fails and the patient has paid full fee for a procedure from which he has derived no benefit. In addition, if the patient chooses to undergo a subsequent VE, the VV has caused some scarring and loss of upper end length in the process of trimming and suturing the upper end, making the subsequent VE more challenging and perhaps less likely to succeed.
One problem with approach number 2 is that all patients pay for the operating room and anesthesia when most would have achieved success in an office environment. When even the most liberal criteria for performing a VE rather than a VV are used (as was done in a recent study), 75% of men in an operating room had a VV on both sides and 8% of men had a VV on one side. Since the VV techniques used in the office and operating room are so similar, these 83% of patients may have enjoyed a return of sperm to the semen at a much lower cost, an important consideration for an operation not covered by most insurance carriers. Another problem with approach number 2 is that after the larger bilateral incisions, patients may take longer to recover than after a single smaller incision and perhaps need more time before returning to work. However, scrotal wounds heal so well that this should not be a major consideration.
(3) A third approach is an attempt to address the problems above. Patients have their procedure in the office. The first step of the procedure is to explore one vas on the testis side of the vasectomy site through a small midline incision. This lower end is opened and the fluid evaluated. If findings are favorable, proceed with VV. If findings are very unfavorable (no fluid or thick fluid with no sperm), no connection is made and for that side the patient is charged an exploration fee much lower than a VV fee. The upper end is left unharmed, there is minimal scarring, and the patient can undergo a VE and sperm harvesting in an operating room at a later date. If the lower end fluid findings are equivocal (watery or thin fluid but no sperm), the patient and doctor can make a decision together about whether to proceed. Then the other side is managed the same way. Most patients, regardless of the interval between vasectomy and reversal, will have favorable findings on both sides, will have a VV on both sides, and will experience a return of sperm to the semen.
Approach number 3 makes the most sense for men whose intervals are short (less than 10 years) and who have no adverse physical findings. Why spend thousands of dollars for an operating room and anesthesia when the likelihood of success with an office procedure is so high? Approach number 2 may make sense when the interval is long. Approach number 1 has, for this practice, provided about half the results summarized in the Results Charts. However, since early 2005, this practice has utilized approach number 3.
Whichever approach is used, vasectomy reversal takes about 3-4 hours. Postoperatively, a dressing is held in place with an athletic supporter. A small soft drain may be left in the scrotum for one to two days to allow egress of blood and thereby prevent swelling.