The most important factor in predicting return of sperm to the ejaculate after vasectomy reversal is the obstructive interval, or duration of time between the vasectomy and reversal. We keep internal records of our outcomes, seen in the below graphs. These may help in a couple's decision process.
On the X axis is "obstructive interval", and on the Y axis is "number of patients." For each year, the lavender bar is the number of men who did have a return of sperm after reversal, and the red bar is the number of men who did not.
The height of the columns is not the measure of success, but just the number of patients at each interval. In general, a "good" result is a high proportion of lavender to red bar height.
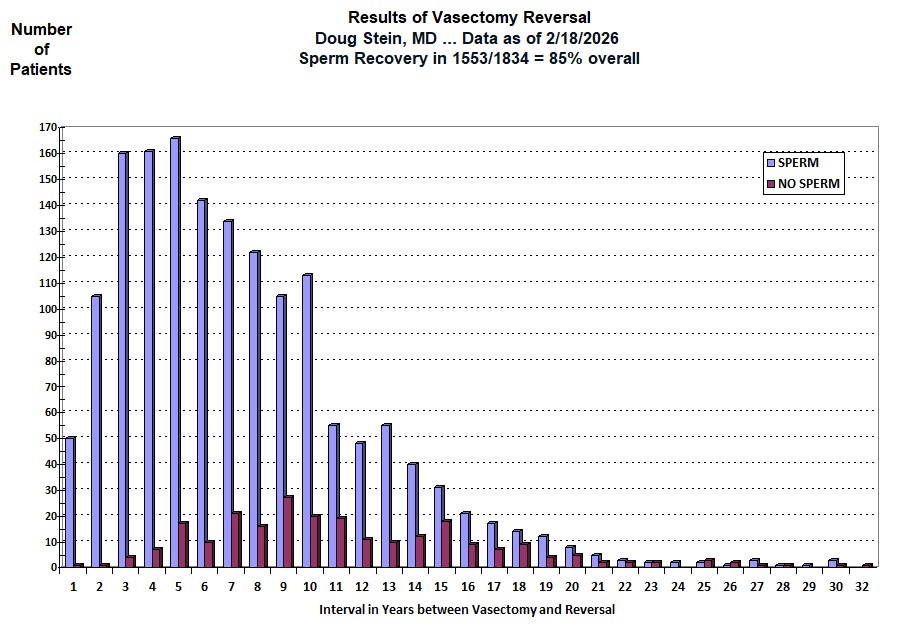
* -The graph above does not include unilateral (one-side) reversals, repeat reversals, and patients who have not yet sent in semen samples. Data for unilateral and repeat reversals is available on request.
** -Not all men represented by the red bars actually underwent full vasectomy reversal. If, at the time of exploration, the lower (testicular) end fluid is poor (creamy or thick, devoid of sperm, packed with white blood cells) on both sides, connections are not performed, the ends are simply dropped back into the scrotum, and the patient is charged no more than his deposit. Yet, he is entered into this database as a "NO SPERM" and "NOT PREGNANT". (It would be a waste of his money to perform connections when the likelihood of success is minimal. That money would be better spent on other options.)
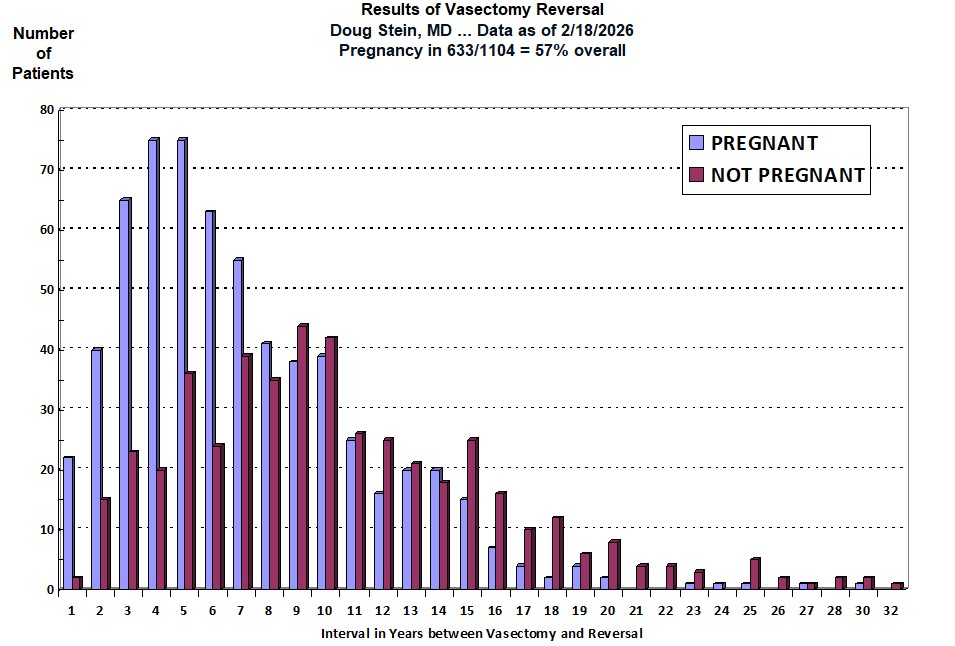
*** - Notice that the number of patients contributing to the pregnancy database is considerably smaller than the number of patients contributing to the sperm recovery database. Almost all patients send or bring in a semen sample after reversal, so sperm recovery rates reflect the vast majority of patients who undergo vasectomy reversal. Couples are added as "NO PREGNANCY" only if it has been one year since the reversal and they have failed to conceive. When we have tried to call our reversal patients who have recovered sperm, we've gotten a variety of responses: "the number has been disconnected," "no-one by that name lives here," "we're separated," "my husband lost his job and money is tight right now so I'm back on the pill," "I got a breast tumor and was told that pregnancy could stimulate my cancer if not fully cured," "we didn't plan on getting pregnant right away, but had you do the reversal to increase our likelihood of success in a few years," "my father died and now I have to take care of my Alzheimer's mother and there is no way I can take care of a baby" and the list goes on. Sometimes we learn about a pregnancy of which we were unaware and another success is added to the data. Sometimes we learn that a couple has been trying for more than a year but sperm density or motility is very low, and another pregnancy failure is added to the data. Sometimes we learn that sperm density or motility is low and the wife has endometriosis or had to have a tube and ovary removed, and we are not sure whether entering the case as a pregnancy failure is justified. Or a patient with a perfectly normal semen analysis gets divorced 9 months after his reversal and his new partner has already had her tubes tied: can't enter him as a pregnancy failure or success. Thus the many reasons for the difference in the total numbers of patients included in the two graphs.
**** - Some couples fail to let us know about pregnancies until we call them. We don't have the time or resources to call all patients with the above delay factors periodically, so there may be more pregnancies than are indicated in the graph above.
In addition, there are no set standards for reporting pregnancy rates. Some offices will enter a couple as a pregnancy failure only if pregnancy has not occurred within two years of the reversal, as opposed to one year as we do. This can make the data "look" better because those couples not pregnant by 18 months after the reversal would not be included in their data as pregnancy failures, whereas they would be included as pregnancy failures in our data. Pregnancy rates will look even better for those offices who do not include couples as pregnancy failures until three years after the reversal ... and so on.
One other point worth repeating ... If the lower end fluid on both sides is of such poor quality that vas-to-vas connections are not performed (because they would be unlikely to result in sperm return to the semen), the patient is entered into the database as a case of "NO SPERM" and "NOT PREGNANT" even though a vasectomy reversal was technically not performed. So many patients represented within the red columns did not have vasectomy reversals. But it is necessary to include them within the data presented to a couple BEFORE we know the quality of the man's lower end fluid.