After vasectomy, sperm are still made by the testes, but they hit the roadblock of the vasectomy site and never exit the body. On each side, sperm can still enter the epididymis (the very long coiled tube behind the testis where sperm mature) and the section of vas below where the vasectomy was performed. After vasectomy, the very fine tubes of the epididymis can become blocked. Blockages in the epididymis occur because white blood cells ingest the trapped sperm, resulting in inflammation. Inflammation can lead to scarring, and scarring in a very fine tube like the epididymis can cause obstruction. The longer the duration of the inflammation, the greater the likelihood of scarring and obstruction. When the epididymis tube is blocked the likelihood of a vas to vas connection being successful is low.
The likelihood of epididymal blockage is roughly proportional to the number of years that have gone by since the vasectomy. After an interval of only 1-3 years, the epididymis is rarely blocked, but after an interval of 20 years, the likelihood of secondary obstruction may be over 50%. Fixing the vas where it was divided at the time of the vasectomy (vasovasostomy or "VV") will not correct the secondary obstruction upstream in the epididymis. That requires a more elaborate procedure called a vasoepididymostomy or "VE", in which the portion of the vas tube above the vasectomy site blockage is connected to the portion of the epididymis "upstream" from the secondary obstruction.
Vasovasostomy (VV) and vasoepididymostomy (VE) are very different operations. The aim of VV is to reconnect the vas above and below where the vasectomy was performed, or reconnect the original tubing. A VV can usually be performed by lifting the vas tubes out of the scrotum through a small hole, just as they were lifted out at the time of the vasectomy. The objective is to freshen the ends on either side of the vasectomy site and suture them back together. Left and right sides can usually be repaired through the same 1/2- to 1-inch vertical incision in the center of the scrotum, all under local anesthesia in a doctor's office. The procedure is performed under magnification using optical loupes or a microscope, 10 -18 sutures are used on each side, and it takes 3-4 hours.
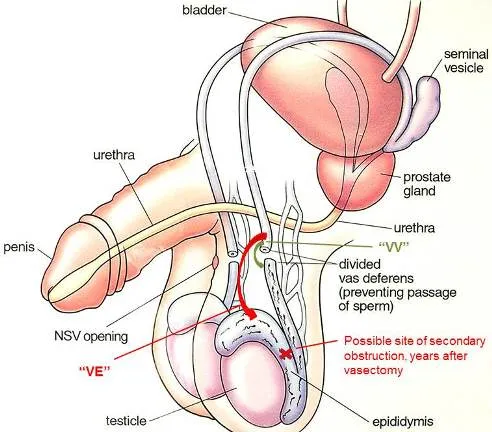
A VE is different in a number of ways. (1) Since the epididymis is attached to the testes, VE requires that the testes be taken out of the scrotum in order to make the connection between the epididymis and vas. This requires an incision larger than that needed for VV. (2) The portion of the vas between the vasectomy site and the epididymis is not used, so the structural gap that must be bridged is longer, requiring that the upper section of vas be "mobilized" to provide the needed length. (3) The epididymal tubes are much smaller than the vas tubes. A microscope must be used, the connection between vas and epididymis (VE) is often not as strong as the connection between vas and vas (VV), and therefore the success rate of VE is not as high as the success rate of VV. The success rate (return of sperm to the semen) with bilateral VE is only about 65%. Because of these factors, VE connections cannot be performed in the office setting.
Many surgeons suggest routinely freezing sperm at the time of VE connections, as a type of insurance plan, in the event that the VE connection is not successful. This way if the VE is not successful, the couple has sperm available for use with in-vitro fertilization. Freezing sperm at the time of VV is much less practical for two reasons: (1) The sperm seen at the time of VV are usually not motile (swimming) and therefore not acceptable for freezing and in-vitro fertilization, and (2) the success rate of VV when sperm are seen coming from the lower end vasal stump is very high.
Ah ... that's the big question. We know that the longer the interval between vasectomy and reversal, the greater the likelihood of an epididymis obstruction. But some men have secondary obstruction after only two years and some do not have it after 30 years. Wouldn't it be nice if we could determine with certainty which men need a VE before they have their surgery? Unfortunately, we cannot definitively know- not by physical exam, ultrasound, CT or MRI.
Physical Exam:
There are a few clues on physical exam: (1) An epididymis that is very enlarged and firm is more likely to be obstructed than one which is small and soft. (2) A nodule (lump) at the vasectomy site may be "sperm granuloma", a place where sperm leaked at the vasectomy site and therefore a "cave" where sperm can accumulate. This area prevents backpressure into the epididymal tubules. So a vasectomy site lump is a good thing, but not all lumps are granulomas ... some are just knots of the suture or clips used during the vasectomy. (3) Some surgeons believe that high (away from the testes) vasectomy sites are a good sign ... more vas on the testis side of the vasectomy site to absorb the back pressure.
Operative Findings:
When the vas is cut below the vasectomy site, we inspect the fluid that drains out. This is a diagnostic step. If the fluid contains sperm, we know that the epididymis and lower vas are open and we proceed with VV connection. If the fluid contains no sperm, especially if it is thick or creamy and packed with white blood cells (pus cells), the likelihood of an upstream obstruction is very high and the likelihood of sperm reappearance in the semen after VV is very low. No fluid at all is a relatively poor sign. Watery fluid, even though devoid of sperm, is a relatively good sign.