This is based upon surveys of our own patients.
Bleeding can occur during or after vasectomy. If this occurs within the scrotum, drainage of a scrotal hematoma (blood clot) in a hospital operating room could be necessary. Smaller hematomas do not require surgical drainage, but tender swelling can last for 2 to 4 weeks. Both large and small hematomas are very rare. If the scrotal skin bleeds at the vasectomy access site, the scrotum can become discolored (black and blue) for about a week; this is more common than swelling, but painless.
Infection is also an extremely rare complication in our practice. Most present as tender swelling and redness of the scrotum and usually respond to a course of antibiotics. In over 50,000 vasectomies, 2 men developed painful walnut-sized abscesses requiring office or operating room drainage through a small incision and a two-week period of local wound care.
Delayed Lightheadedness (fainting) with bodily injury can occur hours after vasectomy even in men who feel great when they leave the office. If a man is driving when this occurs, he could injure himself or others. If he is standing, he could fall and injure himself. We offer all patients a soft drink with caffeine and sugar to decrease the likelihood of this occuring, and we strongly recommend that men come and leave with a driver. Delayed fainting and bodily injury should be considered a risk.
Sperm granuloma is a pea-sized (sometimes tender) lump on the vas tube at the vasectomy site, almost never requiring treatment. Some consider sperm granulomas beneficial, as they may increase the likelihood of success with vasectomy reversal. Periodic tenderness usually responds to an anti-inflammatory medication like ibuprofen, but in over 50,000 vasectomies, 5-10 men been so troubled by chronic tenderness that they chose to undergo removal of the lump, an office procedure performed under local anesthesia similar to the original vasectomy.
Congestion, tender buildup of sperm and white blood cells upstream from or at the vasectomy site, can occur anytime after vasectomy, but usually goes away with use of an anti-inflammatory drug such as aspirin or ibuprofen. Fewer than one in 2000 patients will experience chronic post-vasectomy discomfort (PVPS or Post-Vasectomy Pain Syndrome) severe enough that they will seek vasectomy reversal or neurolysis (division of the sensory nerves coming from the testes). A larger percentage (the American Urological Association says 1-2%) may have milder forms of chronic pain that can affect quality of life but generally not severely enough to seek surgical therapy.
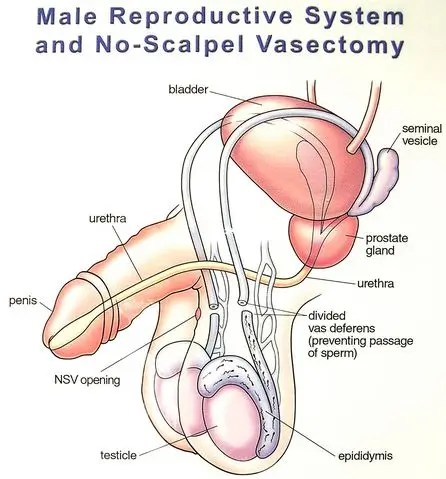
Recanalization is the development of a channel for sperm flow between the two cut ends of the vas. If this happens early during the healing process (within the first few months after the vasectomy) the semen does not becomes sperm-free until the vasectomy is repeated. If recanalization happens late (months or years after a man's semen has been examined and declared sperm-free), an unplanned pregnancy could result; but the odds of this occurring is far less after vasectomy than the odds of pregnancy with any other form of birth control including birth control pills and tubal ligation (female sterilization). Failure rates of vasectomy vary with the technique used to obstruct sperm flow through the vas tubes. In our practice, the early failure rate is about one in 2000 and the late failure rate is also about one in 2000 (details here).
There are no proven long-term health risks (neither cancer nor cardiovascular disease) associated with vasectomy, but since questions have been raised, they are addressed in our page of Frequently Asked Questions.
The risks of NOT having a vasectomy are all borne by the partners of men who choose to avoid vasectomy. And they are considerable!

Since reversal attempts often do not lead to pregnancy, vasectomy should be considered an irreversible form of contraception. Statistics show that men who undergo vasectomy in their 20's are more likely to seek vasectomy reversal than men who have vasectomies later in life. In fact, men in their 20's and with fewer than 2 children should read our Special Message for young men. Before choosing vasectomy, couples, especially couples in their 20's with fewer than 3 children, should consider all other forms of reversible contraception including birth control pills, shots, patches, and implants ; the IUD (intrauterine device); and barrier methods such as the condom and diaphragm, nicely reviewed HERE.
Couples using barrier methods should also be aware that, for those occasions when they are just "careless", EC (emergency contraception, or the "morning after pill") is readily available at most women's health services sites such as private primary care and gynecology offices and Planned Parenthood clinics. EC is effective at preventing pregnancy for up to 72 hours (perhaps longer) after the "careless" encounter.
Men should not proceed with vasectomy if they feel they are being pressured to do so, if their private lives are temporarily unstable due to marital discord, or if they have not considered all reversible alternatives. For many stable men, circumstances change, and all men, especially younger men, should consider sperm storage as insurance against regret over vasectomy in the event of a major life change. If you have never caused a pregnancy, how do we know that you even need a vasectomy ... or what we should expect if you ever opt for vasectomy reversal? Please see our Special Message for Men Who Have Never Caused a Pregnancy.
At our Tampa/Lutz office (click for location and directions), we can usually see any candidate within two weeks.
Because there is so much information here in vasweb.com, especially with the online counseling video, we do not require preliminary consultation visits and most men opt for only one visit, during which we complete the consultation and procedure. If you would like to visit the office and meet Dr. Stein, Galante or Samplaski personally before deciding to proceed, we would be delighted to see you twice. (In fact, we prefer to consult with childless men in their 20's either in person or by telephone at least one week before their vasectomies to thoroughly discuss the issues here.) If the consultation and vasectomy are on separate days, either can be done on any weekday.
All scheduling is done by Heather and Sergio at 813-536-1430 between 9 AM & 4 PM M-F. They can also answer many technical and logistical questions.
As you may have seen in the Florida map on our Index Page, we perform vasectomies at a number of locations in peninsular Florida. A complete schedule with links to maps and information about these locations is in our SCHEDULE page.
You must register online before your visit, but when you arrive, you won't have to fill out all those papers like in many doctors' offices. The benefits are numerous and listed in our On-line Registration Page. Please do not hit SUBMIT more than once. Call our office (813-536-1430) M-F, 9-4 after submitting your registration to arrange a convenient appointment time.
Looking for our Florida vasectomy billboard? Click here